Website still under construction… Skills and Modality Information coming soon.
Therapy Methods
-
Cognitive Behavioral Therapy (CBT) is a structured, evidence-based form of psychotherapy that focuses on the connection between thoughts, emotions, and behaviors. It helps people identify unhelpful or distorted thinking patterns, understand how those thoughts influence feelings and actions, and develop healthier ways of responding. CBT is typically goal-oriented and skills-based, emphasizing practical tools that can be used in everyday life. It is commonly used to treat anxiety, depression, PTSD, and other mental health concerns, and it empowers individuals to build awareness, resilience, and long-term coping strategies.
-
Dialectical Behavior Therapy (DBT) is an evidence-based form of psychotherapy that helps people manage intense emotions, improve relationships, and build effective coping skills. It combines cognitive-behavioral techniques with mindfulness and acceptance strategies. DBT focuses on four core skill areas: mindfulness, distress tolerance, emotion regulation, and interpersonal effectiveness. Originally developed to treat borderline personality disorder, DBT is now widely used for anxiety, depression, trauma, and emotion dysregulation. The goal of DBT is to help individuals create a life worth living by balancing acceptance with meaningful change.
-
Internal Family Systems (IFS) therapy is an evidence-based, trauma-informed approach that views the mind as made up of different “parts,” each with its own role, emotions, and intentions. Rather than trying to eliminate symptoms, IFS helps people build a compassionate relationship with their inner system. The therapy focuses on accessing the core Self—a calm, curious, and grounded state—and understanding protective parts that developed in response to life experiences or trauma. By healing wounded parts and restoring internal balance, IFS supports emotional regulation, self-trust, and lasting change.
-
Eye Movement Desensitization and Reprocessing (EMDR) therapy is an evidence-based treatment designed to help people process and heal from traumatic or distressing experiences. It works by using bilateral stimulation, such as guided eye movements or tapping, while recalling specific memories. This process helps the brain reprocess stored memories so they feel less overwhelming and emotionally charged. EMDR does not require detailed verbal retelling of trauma and is often used to treat PTSD, anxiety, and related conditions. The goal is to reduce distress and support adaptive, long-term healing.
-
Solution-Focused Brief Therapy (SFBT) is a goal-oriented, strengths-based approach to psychotherapy that focuses on solutions rather than problems. Instead of exploring past difficulties in depth, SFBT helps clients identify what is already working and how to build on those successes. Therapists use collaborative conversations, future-focused questions, and small, achievable steps to support meaningful change. SFBT is typically short-term and effective for concerns such as stress, anxiety, and life transitions. The goal is to empower clients to create practical, sustainable improvements in their lives.
-
Acceptance and Commitment Therapy (ACT) is an evidence-based form of psychotherapy that helps people build psychological flexibility. Rather than trying to eliminate difficult thoughts or emotions, ACT teaches skills to accept internal experiences while committing to actions aligned with personal values. It emphasizes mindfulness, present-moment awareness, and values-based living. ACT is commonly used for anxiety, depression, trauma, and chronic stress. The goal of ACT is to help individuals create a meaningful, fulfilling life, even in the presence of discomfort, by choosing actions that reflect what matters most to them.

Understanding Mental Disorders- Psychoeducation
-
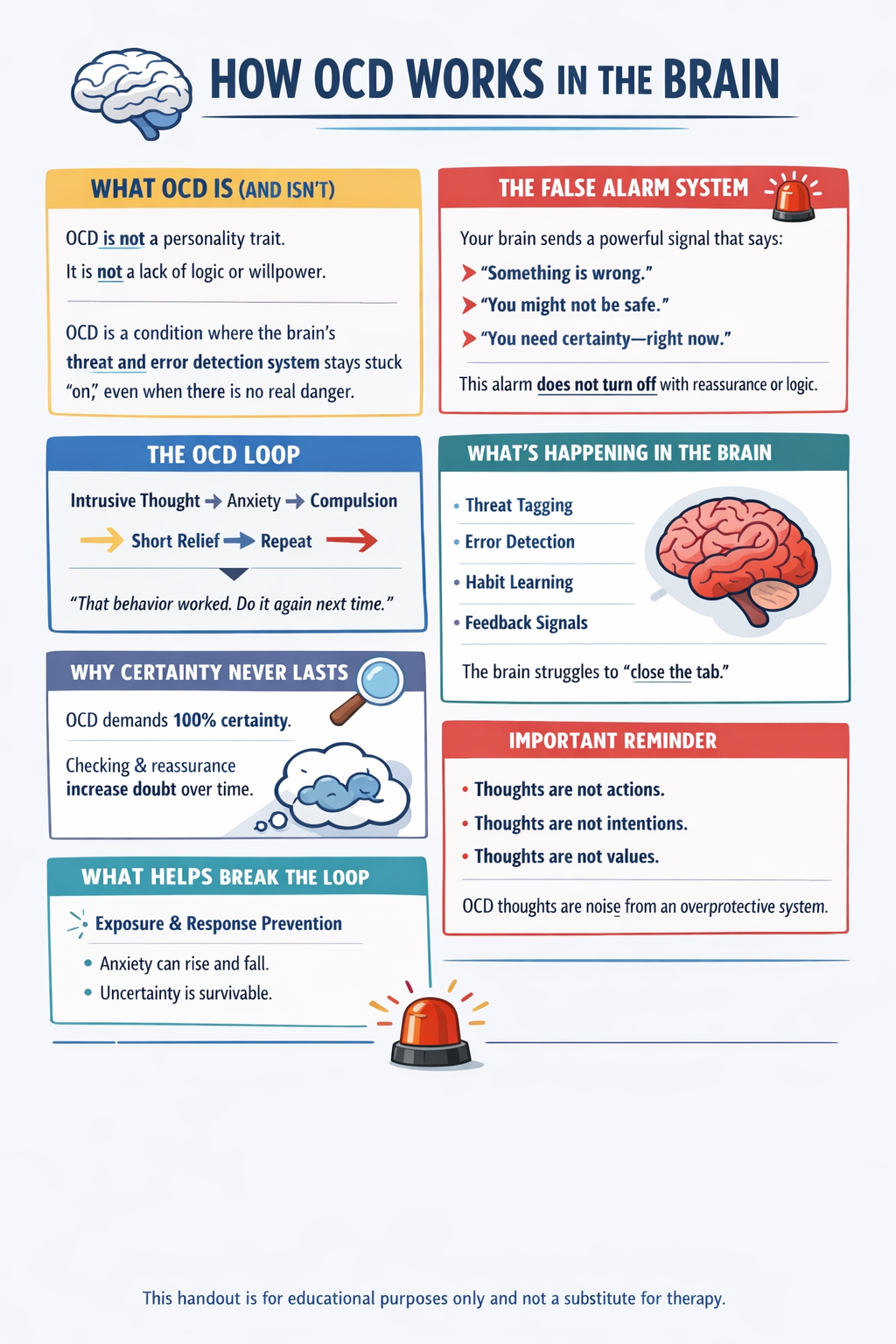
🧠 OCD: WHAT’S HAPPENING IN THE BRAIN
OCD is not a personality trait.
It’s a misfiring alarm system.🚨 The False Alarm
Your brain sends an error signal that says:
“Something is wrong.”
“You might not be safe.”
“You need certainty—right now.”
Even when logic says you’re okay, the alarm doesn’t shut off.
🔁 The OCD Loop
Thought → Anxiety → Urge → Temporary Relief → Repeat
Relief teaches the brain:
“That behavior kept us safe. Do it again.”
This is why OCD feels urgent and sticky.
🧩 The Brain Circuit Involved
(Often called the CSTC loop)
• Threat tagging: marks thoughts as important
• Error detection: keeps saying “still not right”
• Habit system: makes urges feel automatic
• Feedback loop: sends the worry back again and againThe brain struggles to “close the tab.”
❓ Why Certainty Feels Impossible
OCD demands 100% certainty in a world that can’t offer it.
Checking, reassurance, and mental reviewing actually increase doubt over time.🧠 Why Compulsions Don’t Work Long-Term
Compulsions don’t bring peace.
They bring short relief, which strengthens the cycle.Mental rituals count too:
Analyzing
Replaying memories
Reassuring yourself
Googling “just to be sure”
🔓 What Helps Break the Loop
Exposure + resisting rituals teaches the brain:
Anxiety can rise and fall on its own
Uncertainty is survivable
The alarm doesn’t need obeying
The brain relearns safety.
🤍 Important Reminder
OCD thoughts are not your values.
They are noise from an overprotective system.You are not broken.
Your brain just learned the wrong rule. -
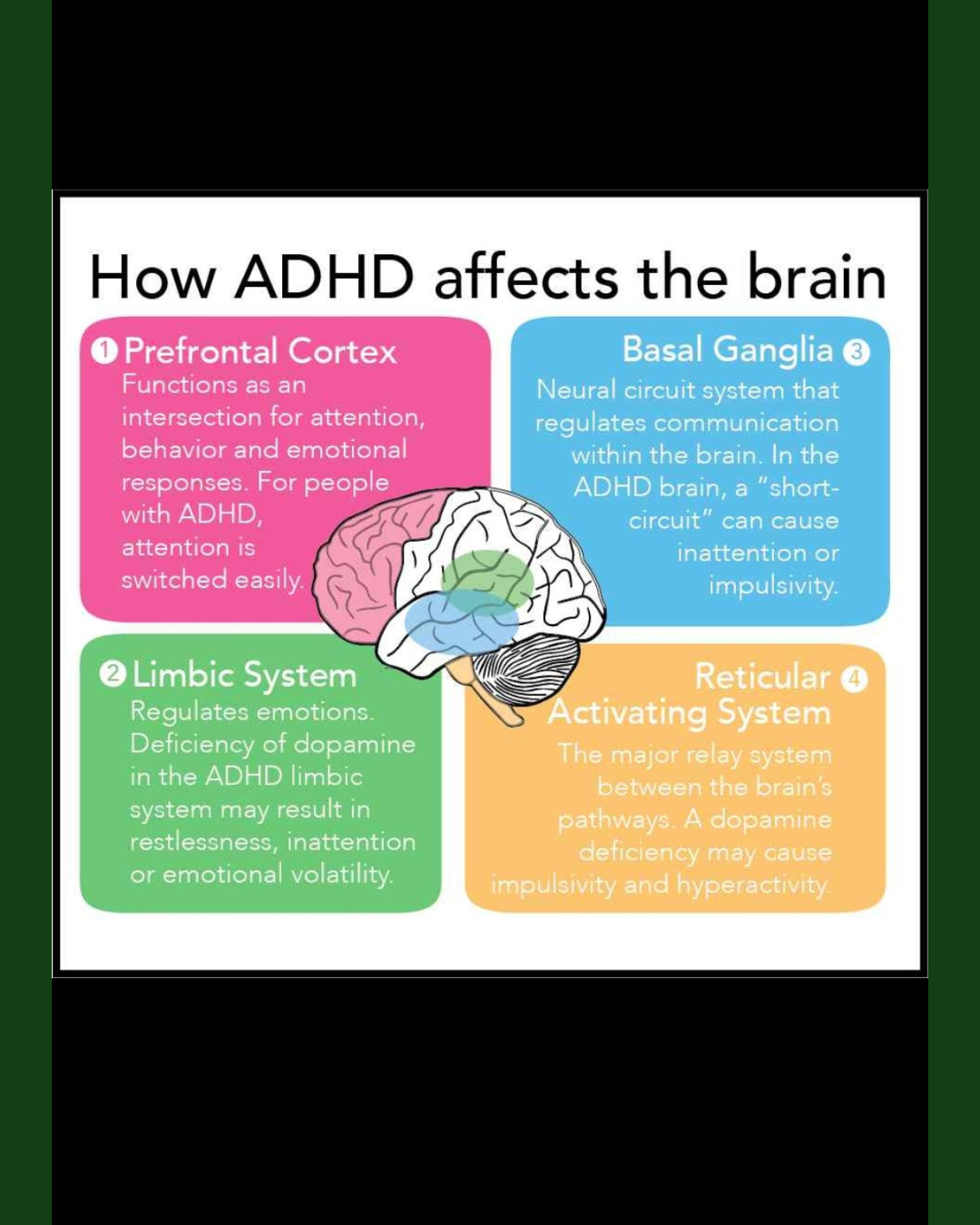
What Happens in ADHD
Research shows three major dopamine-related differences:
A. Lower baseline dopamine levels
• The brain doesn’t release dopamine as consistently
• Tasks feel harder to start
• “Boring” tasks almost feel physically impossible
• People may seek stimulation (movement, urgency, novelty)B. Slower dopamine “reuptake and release” process
• Signals don’t travel as efficiently
• The reward from completing a task doesn’t hit right away
• Can lead to feeling unmotivated even when someone cares deeplyC. Weaker response in the brain’s reward center
The mesolimbic pathway (nucleus accumbens, ventral tegmental area) is less active.
This means:
• Less “reward feeling” when finishing tasks
• Need for more stimulation to feel satisfied
• Hyperfixation when something does spark dopamine -
Depression is more than feeling sad, it’s a medical condition that affects mood, thoughts, and daily functioning. It can impact anyone, regardless of age, gender, or background.
⚠️ Common Signs & Symptoms
Look out for patterns lasting 2+ weeks:
Emotional Changes:
Persistent sadness or emptiness
Hopelessness or guilt
Loss of interest or pleasure in favorite activities
Physical & Behavioral Changes:
Fatigue or low energy
Trouble sleeping (too little or too much)
Appetite or weight changes
Slowed movements or restlessness
Cognitive & Social Changes:
Difficulty concentrating or making decisions
Withdrawing from friends or family
Thoughts of death or suicide
💡 How to Support Someone
Notice & Check-In: Gently ask, “I’ve noticed you’ve seemed down—how are you feeling?”
Listen Without Judgment: Allow them to share at their own pace.
Encourage Professional Help: Suggest talking to a counselor, doctor, or therapist.
Offer Practical Support: Help with everyday tasks, encourage healthy routines.
Stay Present: Let them know they’re not alone.
🚨 When to Seek Immediate Help
If someone talks about self-harm or suicide:
Stay with them until safe.
Call 988 (Suicide & Crisis Lifeline in the U.S.)
Dial 911 if there’s immediate danger.
🌸 Remember
Depression is treatable. Early recognition and support can make a big difference.
You are not alone, and reaching out for help is a sign of strength.
Outside Resources
Need help with groceries, housing, utilities- Click Here
Washington State Department of Youth & Family Services- Click Here
Department of Community and Human Services (DCHS)- Click Here
Washington State Department of Social and Health Services- Click Here
Resources for LGBTQIA+ -Click Here