Learn about different mental health issues.
-
Depression is more than feeling sad, it’s a medical condition that affects mood, thoughts, and daily functioning. It can impact anyone, regardless of age, gender, or background.
⚠️ Common Signs & Symptoms
Look out for patterns lasting 2+ weeks:
Emotional Changes:
Persistent sadness or emptiness
Hopelessness or guilt
Loss of interest or pleasure in favorite activities
Physical & Behavioral Changes:
Fatigue or low energy
Trouble sleeping (too little or too much)
Appetite or weight changes
Slowed movements or restlessness
Cognitive & Social Changes:
Difficulty concentrating or making decisions
Withdrawing from friends or family
Thoughts of death or suicide
💡 How to Support Someone
Notice & Check-In: Gently ask, “I’ve noticed you’ve seemed down—how are you feeling?”
Listen Without Judgment: Allow them to share at their own pace.
Encourage Professional Help: Suggest talking to a counselor, doctor, or therapist.
Offer Practical Support: Help with everyday tasks, encourage healthy routines.
Stay Present: Let them know they’re not alone.
🚨 When to Seek Immediate Help
If someone talks about self-harm or suicide:
Stay with them until safe.
Call 988 (Suicide & Crisis Lifeline in the U.S.)
Dial 911 if there’s immediate danger.
🌸 Remember
Depression is treatable. Early recognition and support can make a big difference.
You are not alone, and reaching out for help is a sign of strength. -
Clinical Definition of Anxiety
Anxiety is a psychological condition characterized by excessive and persistent fear, worry, or apprehension that is disproportionate to actual threat and results in clinically significant distress or impairment in social, occupational, or other important areas of functioning.
From a neurobiological perspective, anxiety involves hyperactivation of the autonomic nervous system, particularly the amygdala and threat-detection circuitry, leading to heightened arousal, increased vigilance, and impaired regulation by the prefrontal cortex. This results in exaggerated threat appraisal and reduced tolerance for uncertainty.
Core Clinical Features
Anxiety disorders commonly present with a combination of cognitive, emotional, behavioral, and physiological symptoms, including:
Cognitive: Persistent worry, rumination, catastrophic thinking, attentional bias toward threat
Emotional: Fear, apprehension, irritability, emotional dysregulation
Physiological: Muscle tension, tachycardia, gastrointestinal distress, shortness of breath, dizziness, sleep disturbance
Behavioral: Avoidance, reassurance-seeking, safety behaviors, compulsive checking, reduced engagement in valued activities
Diagnostic Considerations
Anxiety becomes clinically diagnosable when symptoms:
Persist for a defined duration (typically 6 months or more, depending on diagnosis)
Are excessive relative to situational stressors
Are not better explained by substance use, medical conditions, or another mental disorder
Cause functional impairment or significant distress
-
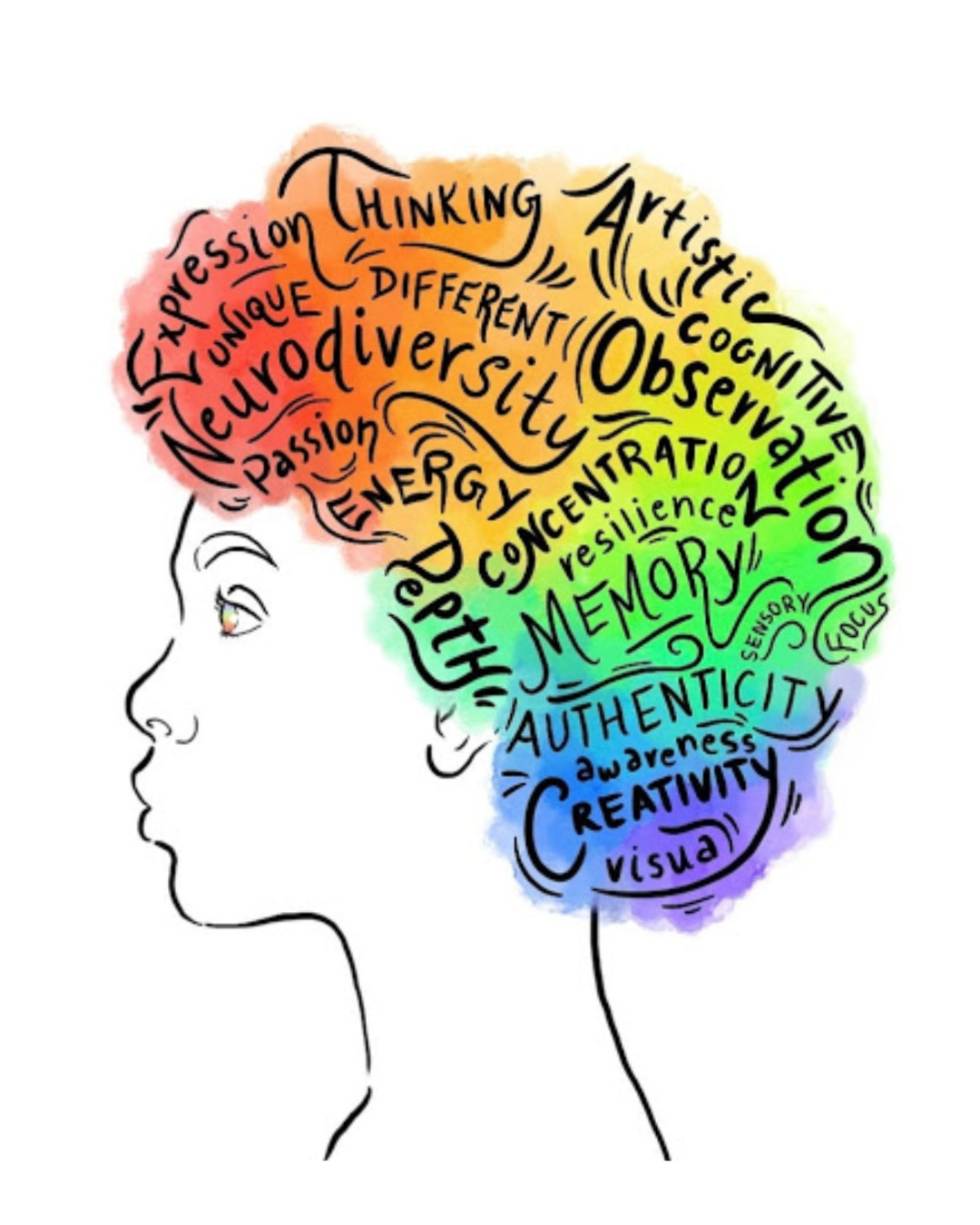
What is ADHD and how does it work?
1. What the Dopamine Pathway Normally Does
Dopamine is a neurotransmitter involved in:
Motivation (“I want to do this.”)
Reward (“That felt good. Do it again.”)
Task Initiation (the spark to get started)
Attention (staying engaged)
Emotional regulation
In a neurotypical brain, dopamine is released in steady, predictable patterns.
2. What Happens in ADHD
Research shows three major dopamine-related differences:
A. Lower baseline dopamine levels
• The brain doesn’t release dopamine as consistently
• Tasks feel harder to start
• “Boring” tasks almost feel physically impossible
• People may seek stimulation (movement, urgency, novelty)B. Slower dopamine “reuptake and release” process
• Signals don’t travel as efficiently
• The reward from completing a task doesn’t hit right away
• Can lead to feeling unmotivated even when someone cares deeplyC. Weaker response in the brain’s reward center
The mesolimbic pathway (nucleus accumbens, ventral tegmental area) is less active.
This means:
• Less “reward feeling” when finishing tasks
• Need for more stimulation to feel satisfied
• Hyperfixation when something does spark dopamine3. How This Shows Up in Real Life
These dopamine differences create what people experience as:
Task initiation struggles (“I want to do it, but I can’t make myself start.”)
Time blindness (dopamine regulates reward + time perception)
Motivation inconsistencies
Procrastination until urgency hits (dopamine spike)
Difficulty with routines (low dopamine tasks feel impossible)
Hyperfocus when dopamine finally locks on to something
Emotion intensity (dopamine interacts with the limbic system)
ADHD isn’t a motivation problem — it’s a dopamine regulation problem.
Neurotypical brain:
Dopamine drips like a steady faucet. Tasks feel doable.ADHD brain:
Dopamine comes in bursts — either too little or too much.
So the brain becomes a “novelty-seeker” to feel regulated.
Therapy Methods
Basic
-
What should we know about the services you provide? Better descriptions result in more sales.
-
What should we know about the services you provide? Better descriptions result in more sales.
Intermediate
-
What should we know about the services you provide? Better descriptions result in more sales.
-
What should we know about the services you provide? Better descriptions result in more sales.
Advanced
-
What should we know about the services you provide? Better descriptions result in more sales.
-
What should we know about the services you provide? Better descriptions result in more sales.